
Pelvic Girdle pain or Symphysis Pubis Dysfunction
Over the past 16 years I have had the privilege of treating many woman suffering with PGP/SPD using classical osteopathic techniques and rehabilitation exercises that are specifically tailored for each patient. I first became interested in the condition, known then as symphysis pubis dysfunction, in 1998 when a mother of two arrived at my private practice with a 15 year history of severe pelvic girdle pain. Her debilitated state had been triggered by the traumatic birth of her second child. I looked up the medical classification of SPD, which read that it was a “self limiting condition related to the pregnancy period”. So why was this patient still suffering from SPD and other related symptoms 15 years later? On examination I found a long-standing pelvic girdle and spinal column misalignment, with associated chronic dysfunctional ligamentous and muscular tissue changes.
I began treating the patient following the principal osteopathic aim of reintegrating the pelvis and spinal column by classical osteopathic articulatory, soft tissue, and adjustive techniques.
It took two years of treatment on a fortnightly basis to relieve the pelvic pain and stabilise the patient’s body, structurally and functionally.
My research showed that there was very little on offer in the way of knowledge or understanding of what causes PGP/SPD how it is diagnosed, and what treatments are available. After 15 years of pain and disability, this patient can now lead a normal life. Had she come earlier for treatment, i.e. before the musculoskeletal compensations became established, the pelvic girdle condition would have been easier to treat and she would have been on her feet quite quickly.
What is PGP/SPD ?
PGP/SPD describes pain in the joints, the ligaments and the muscles that make up the pelvic girdle. The joints include the symphysis pubis joint at the front, the sacroiliac joints at the back, and hip joints at either side of the pelvis. PGP/ SPD is a complex mechanical and functional condition of the pelvic girdle that can manifest symptoms in different sites in and around the pelvis. PGP/ SPD is due to the pelvic girdle struggling to accommodate the structural, functional, and hormonal changes that occur during pregnancy. PGP mainly occurs in pregnancy but has also been shown to occur following a sports injury or trauma to the pelvis.
Signs and Symptoms of PGP/SPD
Pregnancy has the effect of changing the musculoskeletal position and function of the pelvic girdle. Some women’s bodies struggle to adjust to the demands of an increasing weight load upon the pelvis and this gives rise to signs and symptoms of pelvic dysfunction.
Types of pain that can be experienced:
- Acute pain begins suddenly and relieved within three months.
- Chronic pain persists past the normal time of healing for more than six months.
- Aching / sharp / burning / tender / dull.
Location of pain:
- In and around the pelvic girdle: for example, the sacroiliac joints, the pubic symphysis joint, the coccyx, and one or both hip joints.
- The pain can radiate from the pelvis up into the spinal column or down into the buttock and the back of the leg.
- Lower abdomen, groin and perineal area.
- Inner thigh.
- Abdominal pain must always be mentioned at your antenatal check-ups.
Activities that can be painful include:
- Lifting one leg at a time e.g. going up and down stairs.
- Standing on one leg getting dressed or undressed.
- Parting the legs e.g. getting in and out of the car or bath.
- Bending down.
- Turning over in bed / standing / sitting / lying.
- Intercourse.
Intensity of pain:
- Varies from sudden, severe, intermittent pain to constant, chronic disabling pain.
Onset:
- PGP/SPD may begin at any time throughout pregnancy, and/or after labour.
Other Signs and Symptoms
- Clicking within the pelvic joints is common due to the misalignment of the joints and the lax ligaments.
- Bladder dysfunction: stress incontinence, during the last months of pregnancy.
- Sensation that the hip is out of place or has to pop into place before walking.
- Waddling gait.
- Difficulty starting to walk after sleep.
- Round ligament pain: common in the 2nd trimester, by a sharp pain in lower abdomen / hip / groin either on one side or both, caused by sudden movements, including laughing or coughing. Pain should only last a few seconds, and relieved by rest.
- Low back pain.
Hormonal Influence
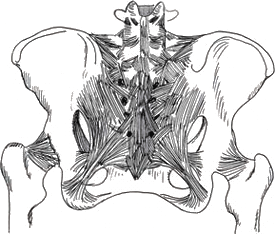
During pregnancy the effects of the hormone relaxin soften the ligaments throughout the body, causing the joints to become increasingly mobile. One of the most dramatic of these changes is the widening and increased mobility of the sacroiliac joints and the symphysis pubis, which begins during the 10th-12th week of pregnancy. Concentrations of relaxin are elevated during the first trimester and then decline early in the second trimester to a level that remains stable throughout the rest of the pregnancy until labour. The pelvic ligaments are bands of tough fibrous tissue that interweave and run in all directions across the sacroiliac and symphysis pubis joints, and with the help of the pelvic muscles they bind the whole pelvis into a single unit. The symphysis pubis joint can separate as much as 9mm in a normal pelvis without problems arising. Problems occur where there is a misaligned pelvis before pregnancy begins. The effect is that the pregnancy hormones potentially create a more vulnerable pelvic base that then struggles to tolerate the added weight-bearing of the advancing pregnancy, manifesting symptoms in one or more of the pelvic joints articulating structures. An unbalanced or rigid pelvis can potentially cause difficulties giving birth and PGP/SPD to develop after the birth.
The pelvis is the main bony weight bearing part of your body and provides the outlet through which your baby is born.
If you are suffering with Pelvic girdle pain it is important that you become aware of and understand how your pelvis is structured and the way that it functions during childbirth so that you can participate in maintaining control of your body throughout the 9 months of pregnancy.
Risk factors
- The hormone relaxin softens the connecting tissue around the joints, making them more flexible in preparation for the birth. This can, however, also complicate the musculoskeletal structures adapting correctly due to an underlying condition that may be causing the maternal body to become unstable and susceptible to stress, strain, or injury.
- Previous pelvic / lower extremity trauma / poor postural development / scoliosis.
- Lax ligaments / weak abdominal muscle tone.
- Previous history of lower back / pelvic / hip pain.
- Increased maternal age.
- Increased number of pregnancies.
- Strenuous work associated with twisting and bending.
- Hypermobility conditions e.g. Ehlers-Danlos syndrome
- Vaginal infection.
- Endometriosis.
- Ovarian cysts
- History of pelvic inflammatory disease.
- Painful varicosities in the legs, vulva or haemorrhoids.
- Rheumatoid arthritis.
- Osteoarthritis of the hip.
Why is the pelvic position so important in pregnancy?
Pregnancy is a time of incredible change within a woman’s body. The pelvic girdle position and condition alone can determine how the posture, spinal curves and centre of gravity alter to accommodate the growing foetus and the extra 20 lb plus of weight. The pelvis plays a key role in maintaining the balance and transfer of weight and movement throughout the body.
Pelvic girdle pain is not a “normal” part of pregnancy if the body is aligned, and most importantly the pelvis has the ability to adapt comfortably to the extra stresses and postural strains of pregnancy. However more than half of all pregnant woman report some kind of musculoskeletal pain.
Pain experienced in or around the pelvis is a sign that the pelvic mechanism is having difficulty adjusting to the new positional and functional demands of the pregnancy.

Diagnosis
Primarily the diagnosis must ascertain and ensure that it is safe to treat with osteopathy. An accurate osteopathic diagnosis of PGP is formulated from a comprehensive case history, a thorough static and dynamic examination of the spinal column, pelvis, posture and gait. Information gathered from this process determines the causative, contributing and maintaining factors that are testing the structural and functional integrity of the pelvic girdle.
Pain experienced within the pelvic girdle can also be caused by numerous conditions, some of which are not musculoskeletal and may not be suitable for osteopathic treatment. In these cases you will be referred to your GP for further tests.
Treatment
The treatment is based on classical osteopathic principles and body mechanics, whereby the osteopathic aim is to integrate and realign the structure and function of the pelvis, the spinal column and all musculoskeletal affected areas. Classical osteopathic treatment is a combination of soft tissue, articulatory and adjustive techniques designed to address the pelvic girdle symptoms by gently coaxing and adjusting the body’s framework enabling the maternal pelvis to stand up to the increasing gravitational stress of the pregnancy. There is also important postural advice and rehabilitation of movement patterns / habits that are exacerbating the problem, i.e. standing / walking / sitting / bending / turning.
Treatment aims and management plans vary from person to person according to the stage of the pregnancy or postpartum.
Treatment may be required every week if the condition is severe, if mildly/moderate once every 2 / 3 weeks until stable.
Treatment given in the latter stages of pregnancy, can in the main, relieve and prevent any further deterioration.
Postpartum PGP/SPD is usually due to an unresolved misalignment of the pelvis that occurred during the pregnancy or to trauma from giving birth. The treatment of women suffering with long-standing postpartum pelvic girdle pain is often more complex because of all the compensatory changes that have developed throughout the body since the onset of the pelvic dysfunction. Classical osteopathic treatment in these cases attempts to evolve the structural and functional compensatory changes back through the way that they have developed, which can in some cases, be a difficult time- consuming process. However don’t let this deter you if you are making steady progress with your practitioner. The process of achieving a full recovery from PGP is not a straight line and it may be challenging at times for both you and the practitioner; as long as you and your practitioner are in agreement that progress is being made, make the most of the opportunity.
It’s important to establish with your practitioner realistic expectations of osteopathic care.
Do not to expect a miracle cure from one treatment, but look for sustained reduction in pain levels, gradually improved mobility and activity levels throughout the course of treatment.
Why is the pelvic position so important in pregnancy?
Pregnancy is a time of incredible change within a woman’s body. The pelvic girdle position and condition alone can determine how the posture, spinal curves and centre of gravity alter to accommodate the growing foetus and the extra 20 lb plus of weight. The pelvis plays a key role in maintaining the balance and transfer of weight and movement throughout the body.
Pelvic girdle pain is not a “normal” part of pregnancy if the body is aligned, and most importantly the pelvis has the ability to adapt comfortably to the extra stresses and postural strains of pregnancy. However more than half of all pregnant woman report some kind of musculoskeletal pain.
Pain experienced in or around the pelvis is a sign that the pelvic mechanism is having difficulty adjusting to the new positional and functional demands of the pregnancy.
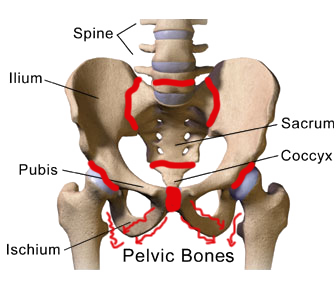
The pelvic girdle consists of :
- 3 bones and 5 joints.
- 2x Sacroiliac joints ( between the sacrum and the two innominates ).
- Pubic symphysis joint ( between the 2 innominates ).
- Sacro-coccygeal joint ( between the sacrum and coccyx ).
- Lumbar-sacral joint ( between the lumbar spine and sacrum ).
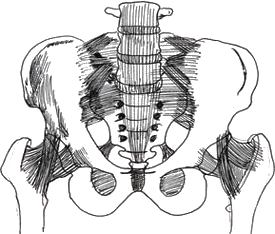
The pelvic joints act and react to one another in response to locomotion, gravitational stress, balance of the spinal curves, and the fluctuating equilibrium between the right, left, front, and back of the body. All these factors determine the positional balance, joint mobility, and interplay between the articulating structures of the pelvic girdle.
During pregnancy the position of your centre of gravity is altered causing the body’s mechanical and physiological balance mechanisms to adjust to this change. Maintaining the integrity of the pelvic girdle during the 9 months of pregnancy is key to providing a stable and adaptable supporting structure for the growing foetus. If the pelvic girdle structure and function is weak or out of balance before pregnancy proceeds, the mechanical equilibrium of the body can become unstable, vulnerable, and more susceptible to stress, strain, dysfunction, and inability to tolerate the increasing demands of the pregnancy.
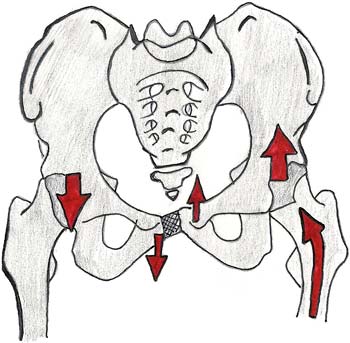
In the majority of patients suffering from PGP/SPD there are common findings:
- The pelvic girdle as a whole has rotated forwards or backwards excessively.
- The right sacroiliac joint has become too mobile.
- The left sacroiliac joint becomes increasingly restricted.
- The right innominate rotates forward and the left innominate rotates backward. This scenario causes a dysfunction of the sacroiliac joint mechanism and the right pubic bone of the pelvis to move down and the left pubic bone to move up, causing a shearing strain in the pubic symphysis joint and ligaments.Each person’s body compensates for these changes in structural balance and mobility in a variety of different ways. Symptoms may range from specific sites of discomfort within the pelvic joints to generalised pain and disability.
Factors that control the postural development during pregnancy include:
- Postural types; anterior / posterior or sway back posture.
- A patient’s morphology: taller, thinner women are more prone to develop an anterior posture
- Shorter, heavier women are more prone to develop a posterior posture.
- Pre-pregnancy state of fitness.
- A small pelvis.
- Previous pregnancies.What ever your postural make-up or movement patterns are, with a bit of awareness of your posture while walking, standing, sitting, moving around, and even lying down can make all the difference to your comfort during your pregnancy or postnatal condition.
How to maintain the correct posture during pregnancy especially if you have Pelvic Girdle Pain.
Pregnancy is a period that undeniably makes demands on your body posture by altering the centre of gravity and weight distribution within your body. This can potentially cause poor postural development or habits to become worse. Developing and maintaining good posture is essential throughout everyday activities in order to reduce the stresses and strains inflicted on the pelvis and throughout your body.
Essentially a conscious effort is required to improve and maintain the balance between the pelvis, abdomen and thorax. Establishing pelvic girdle control is vital so that you can evenly distribute the gradual increase of weight and reduce any antagonistic muscle action developing in and around the pelvis, thus enabling the legs to move without restrictions or compensation.
A common mistake many pregnant women make is to let the weight of the bump rotate the pelvis too far forwards. The lower back then arches forward excessively and locks up the lumbar/pelvic joints, resulting in too much front heavy stress and strain on the symphysis pubis joint.
The other common presentation is when the pelvis rotates backwards excessively, which leads to too much pressure accumulating within the pelvic cavity and straining of the pubic symphysis joint and ligaments from inside the pelvis, pushing out.
For a woman diagnosed with PGP/SPD it is important to become aware of the way you are standing and moving your body which could be causing, aggravating or maintaining the condition.
As a general rule of thumb, the majority of the maternal body’s mechanical adjustments tend to diminish after the 28th week of pregnancy, so if you have not experienced any PGP/SPD up to this stage the chance of getting the condition reduces considerably.
However, late in pregnancy a woman may experience pain in the pubic area as the pubic joint begins to widen in readiness for the birth. If this is happening to you, avoid all strenuous exercise and positions which worsen the pain.
Women used to keeping fit should bear in mind that pregnancy is a time to adjust their fitness programme to an appropriate level. It should be neither over strenuous, straining, nor tiring.
Prognosis
After many years of researching and treating PGP/SPD there is now sufficient evidence to show that classical osteopathy, coupled with rehabilitation exercises, can make a considerable difference to women suffering with PGP/SPD. This is supported by many testimonials and the steady increase in the number of referrals directed to the Tunbridge Wells Osteopathic Practice.
Help and support
Do not forget that there is additional help and support out there if you need it during those
challenging and testing times along the journey. Getting the help and support you need
can make recovery times much quicker.
NCT helpline www.nct.org.uk
Independent midwives www.independentmidvives.org.uk
Doula www.doula.org.uk
Pain concern uk www.painconcern.org.uk (provides information and advice to chronic pain
sufferers)
Counselling and emotional support www.bacp.co.uk
Citizens advice bureau www.citizensadvice.org.uk (advice on benefits)
Disability, pregnancy and parenthood www.dppi.org.uk
Carers centres www.carers.org
